April 24, 2020 | Posted by MICRO
Introduction
The restoration industry has extensive experience in assisting individuals and organizations when their lives have been disrupted by catastrophic events such as floods and fires. Therefore, it is no surprise that clients are turning to restoration professionals to assist them in properly responding to the coronavirus pandemic referred to as COVID-19. In such circumstances it is imperative that restoration professionals be clear about what their services can, and cannot, accomplish for the client.
This document has been prepared by a wide range of experts from the cleaning and restoration industry to assist contractors in managing the risks arising from efforts to mitigate the COVID19 pandemic. This Preliminary Report is based on extensive industry experience and, to the extent possible, we have incorporated guidance provided by the Centers for Disease Control and Prevention (CDC) and the U.S. Environmental Protection Agency (EPA), as of the published date of this document. While each project is unique and requires a specific work plan, restoration contractors may consider the information contained in this document to formulate their work practices.
However, this Report is preliminary, and should not be construed as, an industry standard. This is a rapidly evolving situation and more research is needed. At this point in time, it is not feasible to write definitive rules that will apply to every scenario. In certain situations, deviations from these methods may be appropriate, based on the circumstances of the project and the professional judgment of the professionals involved. Common sense should prevail in all cases. This Report is intended solely for informational purposes to supplement the training and other research performed by the restorer and is not to be construed as advice.
Anyone using this document should understand the document’s limitations, and rely on his or her judgment, or as appropriate, seek the advice of a competent professional in determining the exercise of reasonable care in any situation. All persons using this document must be and remain, updated and informed about developments pertaining to COVID-19 and the restoration industry so that he/she may implement changes in procedures as appropriate, as well as adhere to all applicable federal, state, provincial and local laws and regulations.
Disclaimer
RIA and IICRC make no representation or warranty as to, and are not responsible for, the contents, validity or application of the information by any recipient of this document. RIA does not warrant that the information in this document is free of errors and the entire risk of the use of any information in this publication is assumed by the user.
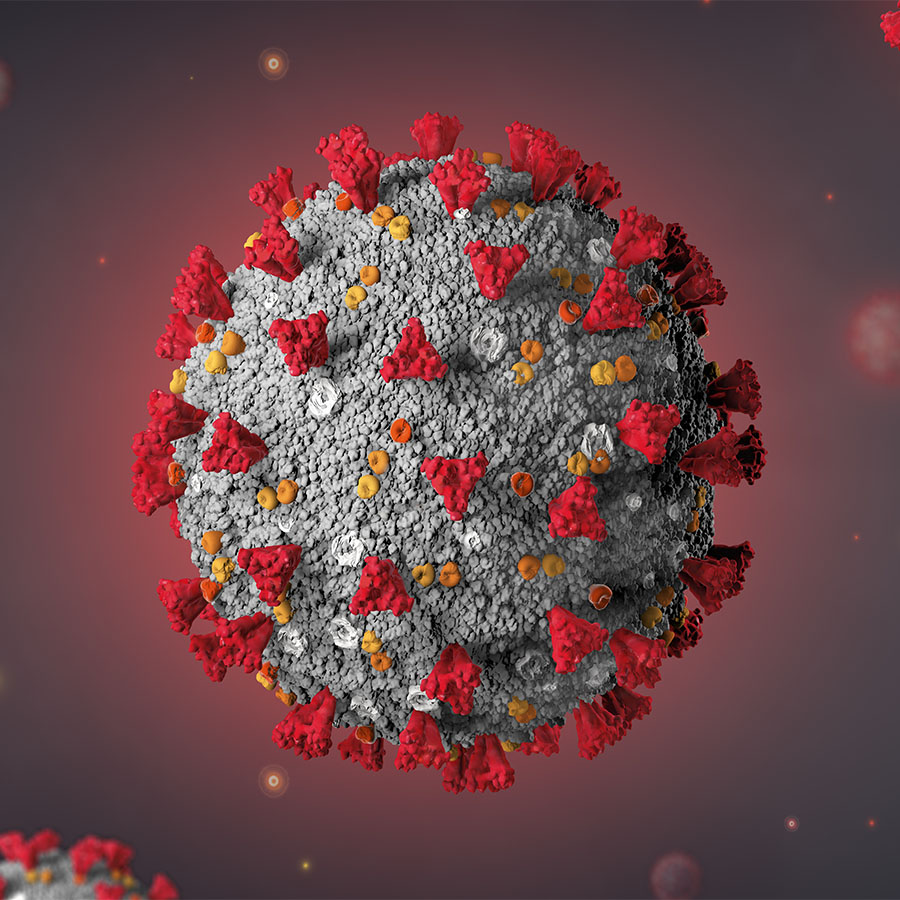
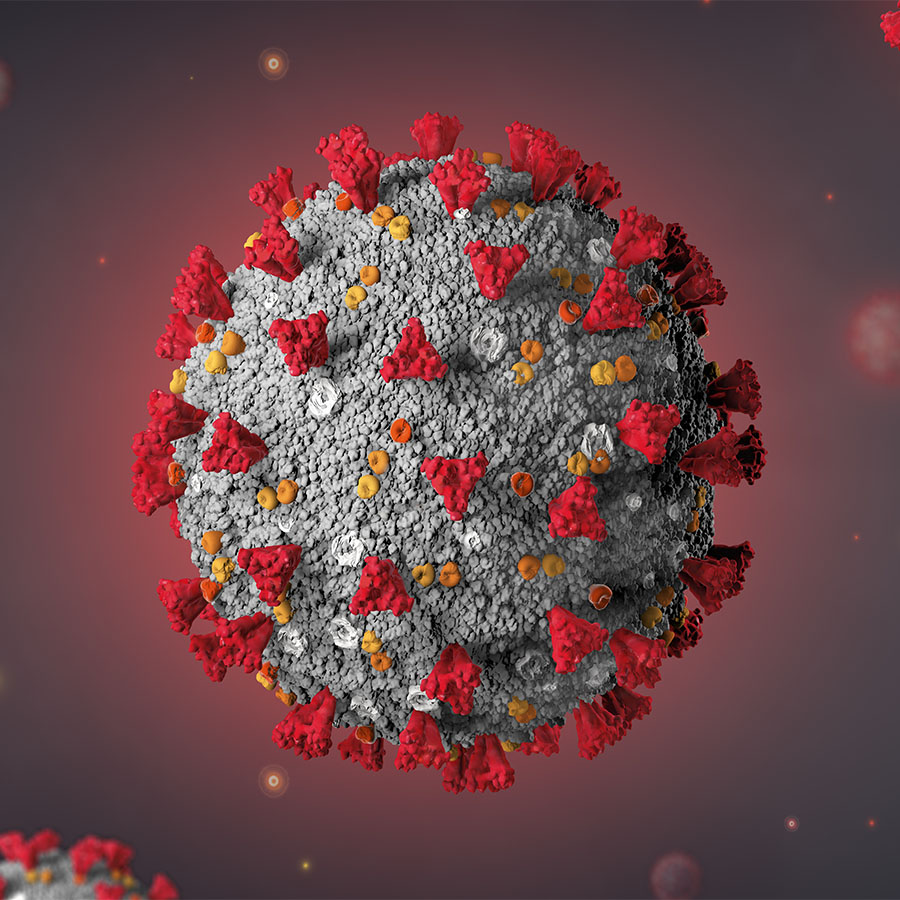
Basic Information About Coronavirus
Coronaviruses are a type of organism that often cause respiratory diseases in people and animals. In the fall of 2019 a new mutation of a coronavirus was first detected in China. The new variation was soon recognized to have properties similar to the 2003 coronavirus that led to the description of Severe Acute Respiratory Syndrome (SARS). As such, the virus was named “SARS-CoV-2” by the World Health Organization (WHO). Exposure to SARS-CoV-2 can lead to a specific form of illness characterized by very high fever and dry cough named “coronavirus disease 2019” – abbreviated “COVID-19”.
Within months of its identification, despite extensive efforts at containment, COVID-19 spread around the globe and was declared by the World Health Organization to be a “pandemic”; a world-wide epidemic of an illness for which people have no natural immunity. To address the risk, significant efforts are being directed at developing a vaccine. However, as of the published date of this document, no such preventative medicine is available. According to the Centers for Disease Control and Prevention (CDC) “Nonpharmaceutical intervention would be the most important response strategy” to COVID-19. Their pronouncement means that infection control and home care of the affected are the key response measures.
It is noted that older adults, particularly those with weakened immune systems and underlying health problems, are at a higher risk for severe COVID-19 associated illness. This means that medical facilities and eldercare accommodations are especially vulnerable to outbreaks.
Infection Control Principles
Decades of scientific studies and practical experience have shown that effective control of infectious agents in the population requires a nearly equal combination of adjusting people’s behavior and taking additional steps to stop the spread of contamination from surfaces. This dual approach to infection control is necessary for COVID-19, as the best available information indicates that it is spread both by direct exposure to the droplets aerosolized when an infected individual coughs or sneezes and by secondary exposure of uninfected people to objects and surfaces with residual viral particles.
Secondary exposure is likely more of a problem with COVID-19 than the normal flu as some early reports from the CDC indicate that the virus may remain viable on nonporous surfaces for up to nine days as compared to one-three days for normal influenza viruses.
The recommendations in this document are designed to address secondary human transmission through the cleaning of facilities to prevent the spread of the virus from surfaces within buildings. While the exact extent of disease transmission from contact with surfaces is currently unknown, initial indications are that prolonged exposure to contaminated surfaces does lead to higher infection rates. Therefore, cleaning surfaces and applying a disinfectant are important risk mitigation techniques.
During past viral outbreaks the behavior component of the infection control process has been voluntary. Individuals are reminded to stay home if they are sick, educated to cover their cough and sneeze, and encouraged to wash their hands frequently. This voluntary approach has been supplemented with CDC suggested cancellations of activities that would bring large numbers of people into close proximity; including closure of schools, colleges, sporting events and amusement venues. Containment efforts have also resulted in authorities closing bars and restaurants in many states, along with enactment of international travel restrictions.
While these measures to adjust behavior will hopefully slow the spread of the virus, such efforts need to be matched with practices proven to minimize secondary transmission. Restoration contractors must emphasize to their clients that actions taken to reduce exposure from secondary transmission from surfaces with reservoirs of viral material must be matched with procedures to prevent recontamination. Cleaned and treated surfaces can become recontaminated in minutes if an infected individual is present and sneezes or coughs without controlling the droplet spread.
Potential Services
With the proper training, equipment, supplies and personal proactive gear, restoration contractors who have experience dealing with other hazardous microorganisms, such as sewage mitigation and mold remediation, can offer valuable services to combat COVID-19. The most basic service will likely be enhanced cleaning of touchpoints and application of disinfectants to other surfaces. It is important that the restoration contractor communicate clearly and use consistent terminology when describing the services. Because no currently available antimicrobial has been tested against the SARS-CoV-2 (see section below on Pre-work Preparations for additional details), it is important to use the verbiage to “clean and apply disinfectant” rather than “clean and disinfect.” With no validation of a product’s effectiveness for this particular virus, there is no way for the contractor to know if the appropriate level of microbial reduction has been reached in order to meet the definition of the term “clean and disinfect”. As such, contractors are offering a service to clean and apply an appropriate EPA registered disinfectant in accordance with the application directions provided by the master label.
Even with that distinction in language, it is clear that the cleaning of touchpoints and specialized treatment involving application of disinfectant is an essential service. If demand for such services grows beyond the capacity of the restoration contractor, consideration should be given to partnering with the client to educate existing custodial staff on proper techniques for cleaning touchpoints after which the restoration contractor can provide the specialty treatment of applying disinfectants to surfaces.
Other services that the restoration contractor may be able to provide to clients in the medical and eldercare industries include temporary isolation of rooms or areas to create negative pressure treatment or quarantine spaces. Contractors providing these services to medical facilities should be familiar with Infection Control Risk Assessment (ICRA) guidelines. Although ICRA guidelines apply specifically to contractors conducting construction activities, they provide important guidance on infection control measures. HEPA vacuuming and the use of HEPA filtered equipment such as air scrubbers can also improve the environment by reducing the level of airborne particulate. The removal of aerosolized particulate during the cleaning process may further improve the overall cleaning efficacy and reduce risk.
With the recent announcement by the CDC that the virus can likely be transmitted through contact with contaminated clothes, linens, and shoes, the washing of soft goods now has increased importance. Restoration contractors who want to offer these services should use the CDC guidelines as a baseline for this work.
Pre-work Preparations
Restoration contractors should only offer services to assist with the control of COVID-19 if they are suitably prepared with the proper training, equipment, and insurance to perform these services and have experience in dealing properly with other biological contaminants. Given the rapid developments surrounding this situation it is essential that restoration contractors review their current insurance policies to determine if they have proper coverage. Even those companies that have endorsements to cover mold or sewage work may need additional policy enhancements depending on the definitions in their general liability and adjunct insurance binders.
At a minimum, contractors should review their general liability, contractor’s pollution liability, professional liability, and workers’ compensation policies with an experienced agent or broker to determine if:
- There is a communicable disease exclusion;
- There is a separate exclusion for virus or microbial matter;
- The cleaning and applying of disinfectant constitutes a material change in the insured risk;
- The cleaning and applying of disinfection for viral control is specifically covered, or at least not specifically excluded;
- The full scope of offered services is covered.
A thorough review of company policies related to site risk assessment, use of personal protective equipment (PPE), and infection control work practices is critical. American, Canadian, Australian and New Zealand regulatory agencies, among others, require employers to protect
their workers from a “recognized hazard”. This means that employers are responsible for taking reasonable steps to protect their employees.
Any respiratory protection assigned to crew members who will perform touchpoint cleaning or surface treatment, including filtering facepieces such as an N-95 mask, must comply with regulations established by authorities having jurisdiction such as OSHA, Health Canada, Safe Work Australia and Worksafe NZ. Typically, regulatory requirements include employee medical evaluation, fit testing, training, and a written program. In contrast, providing surgical style masks to potentially infected individuals to control the spread of sneeze and cough droplets prior to their departure from the worksite does not constitute giving them a respirator; an action that triggers compliance with respiratory protection regulations.
Providing services in workplaces and public buildings generally requires a basic risk assessment to protect workers from biological, chemical, and safety hazards. In contrast, work performed in food service establishments requires compliance with numerous food safety regulations and generally requires the use of disinfectants that are appropriate for such operations. Many state and provincial regulatory agencies, as well as facility specific rules, require training and/or certification to assist with cleaning and sanitization activities in healthcare facilities.
The crisis nature of the COVID-19 response means that many typically available supplies may now be in short supply. This may require contractors to use alternate personal protective equipment (PPE) items they are not familiar with, or potentially reuse single use products. As an example, the CDC has already posted procedures explaining how personnel may have to store and reuse single use disposable respirators. Contractors may have to use different personal protective equipment (PPE) than what they are used to. Shortages of disinfectants may also occur.
Choosing a sanitizing product can be confusing as the sudden onset of the SARS-CoV-2 virus means that commonly used antimicrobial products have not been tested or have not received a U.S. Environmental Protection Agency (EPA) registration specifically for cleaning surfaces with viral materials that cause COVID-19. In this situation, the EPA falls back on its “emerging pathogens program” to provide guidance in evaluating a product’s effectiveness in arresting the spread of the virus. Their guidance on the best practices to break the chain of infection when new microbial threats appear allows companies with existing registrations that document product effectiveness in killing similar organisms to utilize those chemicals against the new threat. Therefore, any products used by restoration contractors should be listed on the EPA “Emerging Pathogen/List N” or meet the requirements of the emerging pathogens procedures for enveloped viruses (the class of organism of the SARS-CoV-2). It is critical that restoration contractors understand that the “List N” is not exhaustive, does not represent any EPA endorsement of listed products, and changes repeatedly as products that are not currently listed demonstrate similar effectiveness.
It is important to note that equipment must be scrupulously cleaned between each project. Contractors should validate their equipment cleaning procedures to ensure that no microbiological contaminants will be transferred from one location to another.
Crew Safety
The minimum personal protective equipment (PPE) recommended by the CDC for individuals potentially exposed to COVID-19 includes gloves, gowns, eye protection, and respirators. Typically, workers in the restoration industry use disposable suits with attached hoods and booties for contaminant control work.
However, if a shortage of disposable suits occurs, disposable lab coats or full front treatment gowns with long sleeves that tie in back could also be used for body covering. Depending on the availability of disposable suits, workers may have to utilize reusable medical style scrubs consisting of top, pants, cap, and shoe covers. Such outerwear can be worn as a replacement for street clothes if a controlled changing area is available or purchased oversized and worn on top of street clothes. In such cases proper provisions for the collection, handling, and cleaning of clothes are necessary.
For most work conducted by restoration contractors related to mitigation of COVID-19, CDC and Health Canada recommend an N-95 filtering face piece as minimum protection against possible exposure to the viral contaminants. Out of an abundance of caution, an N-100 is recommended for restoration contractors in situations where airborne contamination may be extensive due to the existing conditions or cleaning methods employed. If filtering face pieces are used, a full-face shield rather than safety glasses can be used in order to minimize fogging and to protect the eyes from exposure to potential contaminants. A full-face negative pressure respirator with HEPA filters can be used to provide respiratory and eye protection in one device. A greater level of protection is provided by a mask or hood style powered air purifying respirator (PAPR). Respiratory protection must also be matched to protect workers from the chemicals used when applying disinfectants to the surfaces.
Regardless of what particular personal protective equipment (PPE) is used to protect workers, it is necessary to train them how to use it properly. This includes the correct methods of donning and doffing the equipment. Because small actions can be important to protect workers and minimize the spread of infectious agents there are even proper, detailed, procedures for removing surgical style gloves.
Contractors should emphasize to their crew members and clients that helping stop the transmission of COVID-19 is serious work and does carry some risk. Therefore, all safety and health procedures must be followed without exceptions.
Cleaning of Touchpoints
The first step in cleaning and sanitizing to break the chain of COVID-19 illnesses from secondary surfaces is to remove soil and other surface contaminants. Emphasis should be placed on cleaning surfaces more likely to be touched by occupants; commonly referred to as touchpoints. Since people are not precise when touching objects, touchpoint cleaning should extend past the focused item 3-12 inches. Common touchpoints include, but are not limited to, door knobs and locks, door push bars, door edges and jambs on the side opposite the hinges, stair and ramp hand railings, cupboard handles and drawer pulls, appliance handles, light switches, table and desktops, telephones, toilet seats and flush handles, faucet handles, soap pumps, keyboards and mice, elevator buttons, credit card keypads, vending machine buttons, equipment controls, television remote controls, chair armrests, bedrails, and countertops.
Touchpoints will also vary by the type of facility being cleaned. Pew tops and armrests, communion rails, confessional kneelers, altars, and holy water dispensers are touchpoints that need cleaning in churches. Toys, books, and teaching supplies will need attention in schools. Medical facilities will require an additional focus on wheel chair handles and wheel grips, computer stations, IV poles, divider curtains, blood pressure equipment, bed stands, food delivery carts, laundry and trash containers, and nurse call buttons. While not a touchpoint that typically gets addressed by the restoration contractor, clients should be advised to remind occupants to frequently clean their cell phones and other mobile devices during pandemics and times of increased disease transmission.
Typically, a trigger sprayer and a wiping cloth are used for cleaning most touchpoints. In that circumstance, spraying the cloth and then wiping is preferable to spraying the surface. If it is an allowable application method under the EPA registration for the particular chemical, substituting pump up devices that deliver the chemical product as a foam is a technique that has multiple advantages over a sprayer for cleaning touchpoints. A foam application allows the worker to see what has been covered, allows the product to stay on the surface longer without drying, and uses significantly less of the cleaning product. For facilities with a large number of desks, tables, or counters, using a foam applicator and squeegee to remove the residue into a rag or disposable towel is another efficient cleaning method.
The specific examples provided in this section should not be considered the best methods as each situation presents its own challenges. Each project should be evaluated for procedure and methods that are appropriate to meet the goals of the client. Proper touchpoint cleaning includes developing a facility specific checklist of critical touchpoints, providing the checklist to workers with training on the particular products and application methods to be used, and allowing adequate dwell time for the cleaner/sanitizer. Additionally, appropriate supervision of the cleaning activities, as well as post cleaning evaluation (see section below on Post-work Project Evaluation for additional details) must be part of proper touchpoint cleaning.
Applying Disinfectants
Cleaning touchpoints is crucial to reducing the spread of COVID-19. To further reduce the potential for infection transmission, touchpoint cleaning should be paired with the application of disinfectants to the many surfaces where viral contaminants may exist. Applying appropriate antimicrobial solutions as an aerosol is an effective way to reduce microorganisms on walls, floors, and horizontal surfaces. Caution should be used to assure that the materials and methods used are compatible with the uses of the building and any rating the structure has obtained for energy or environmental efficiency.
There are numerous processes and systems that can be effective in completing large area sanitization. Many antimicrobial products currently used in the restoration, medical, and food service industries can be utilized by adjusting the application method from trigger sprayer to pump sprayer, misting equipment, airless sprayer, electrostatic sprayer, ultralow volume (ULV) fogger, or thermal fogger. Prior to the selection of any alternate application method review the product label (not just the Safety Data Sheet or use instructions) to confirm that the product is registered for that application method.
Antimicrobials and disinfectants can be used if approved by the EPA or the U.S. Food and Drug Administration (FDA) for the purpose of surface sanitization and/or listed on the EPA “Emerging Pathogen/List N” or meet the requirements of the emerging pathogens procedures for enveloped viruses (the class of organism of the SARS-CoV-2).
Several steps should be completed prior to the broadscale application of disinfectants to surfaces. Return air vents should be covered to prevent migration of the disinfectant into the equipment or to other areas. While air duct cleaning can be incorporated into COVID-19 response procedures, the EPA has strict rules regarding which products can be used in HVAC systems. It is also at this time not clear that the HVAC or air conveyance system plays a role in the spread of SARS-CoV-2 virus, and the inclusion of HVAC cleaning and decontamination therefore may not be necessary. Opening doors or windows to reduce the level of airborne droplets is recommended by the CDC. Setting up HEPA filtered negative air machines as air scrubbers can reduce the airborne particulates that get dislodged by the treatment process.
After selecting an approved combination of disinfectant product and application method, the prepared disinfectant should be applied in accordance with label directions. Depending upon the facility and specific space, when walls are considered a potential touchpoint, wall surfaces should be included in the application of the disinfectant. Shelves, bookcases, file cabinets, or other fixtures may require a higher starting point. Application should begin at the designated upper height and move down to floor level in overlapping passes to ensure that every part of the surface to be treated is adequately covered.
Depending on the listed product dwell time and the application method, the disinfectant may be able to be applied once or it could require multiple treatments to keep the surfaces wet for
the minimum time. Careful assessment of the surfaces will be necessary to prevent the product from streaking or running while keeping the surface wet for the recommended contact time.
Floors and other horizontal surfaces should be treated after the product has been applied to all walls. Floor surfaces should be free of visible debris before treatment. In most cases, HEPA vacuuming of the floor surface will remove the majority of visible debris. Regular vacuuming, dust mopping, or sweeping is not recommended when cleaning to prevent COVID-19. Disinfectant should be applied to floors in a pattern that allows the operator to finish at an exit without having to walk over the wet floor.
Post-work Project Evaluation
The combination of touchpoint cleaning and application of a disinfectant to other surfaces is a proven strategy to break the chain of infection. Although these efforts are designed to affect microorganisms that are too small to see without magnification, a detailed post work visual inspection is still the first step to evaluate the effectiveness of the efforts to control COVID-19. A white cloth should be wiped over representative touchpoints that have been cleaned and should not reveal any discoloration or residue. Any visible debris deposited on the cloth (not disinfectant residue) indicates a need for recleaning of all touchpoints represented by the sample.
If desired by the contractor or the client, analytical methods can be used to supplement the visual inspection. A useful process that provides on-site results is a swab collection of surface samples using an adenosine triphosphate (ATP) meter. ATP meters do not identify viral contaminants since those organisms do not produce ATP. However, the overall reduction in biological contaminants is an excellent surrogate measure of cleanliness since selective cleaning of specific contaminants is impossible (e.g., it is not possible to clean bacteria and leave behind just the virus).
Given the ability of ATP to measure general biological residue, representative testing using an ATP meter can be conducted if additional assurance of project effectiveness is necessary. Sample results should be compared to guidelines for hygiene surface testing provided by the manufacturer of the specific ATP meter. Another approach to documenting the effectiveness of the process is to utilize the ATP meter on a number of representative touchpoints prior to the start of cleaning and again at the end to compare the level of reduction that was achieved.
Project Documentation
Regardless of the technology and chemistry used for touchpoint cleaning and surface sanitization treatment, the restoration contractor must document the work to confirm that it was completed correctly. Project documentation for COVID-19 activities should include a written description and photographs of any isolation barriers set up as part of the cleaning and sanitization process.
Specific personal protective equipment (PPE) for workers should be documented. Records should also be kept regarding the specific equipment used for chemical application, including the process that was used to clean the equipment prior to adding the selected antimicrobials. These records should confirm how the product was mixed if it was not a ready-to-use cleaner/sanitizer. The correct application rate is another crucial data point to be documented. Evidence of appropriate dwell time, as noted from the product label, also needs to be recorded. Finally, if the cleaning/sanitizing product requires rinsing or neutralization, the procedures to comply with that requirement should be fully explained.
Acknowledgements
RIA would like to thank the following individuals who contributed their time and expertise to the development of this document; especially to SERVPRO for their financial support for this industry wide effort. Michael Pinto, FLS, CSP, CMP, Wonder Makers Environmental, the Chairperson of the RIA’s Environmental Council was the primary author of this document. Contributors included: J. Scott Armour, M.S., Armour Applied Science; Kristy Cohen, Restoration Industry Association; David Dybdahl, CIC, CPUC, ARM, American Risk Management Resources Network; John DiMenno, CR, CMRS, CMP, WLS, Romualdi Davidson and Associates; Norris Gearhart, CR, Gearhart and Associates; Mark Meece, Complete DKI; Tom Peter, Insurance Restoration Specialists; Kent Rawhouser, CMP, WLS, A&J Restoration Services; and Shawn Silliman, CR, WLS, First Restoration Services. Reviewers included: Hugh Crisp, BluSky; Dr. Halden Shane, Sterimist; Bruce White, SDS Forensic Laboratory; Graham Dick, Infection Control Training Group and IICRC S410 Infection Control Consensus Body Chair; Mark Drozdov, IICRC Director and IICRC S410 Infection Control Consensus Body Vice Chair; Brandon Burton, Next Gear Solutions; IICRC Standards Chairman; Lee Senter, CEO of Dryit.ca and IICRC Standards Vice Chair; and Edward H. Cross, Esq.
Copyright March 19, 2020 by Restoration Industry Association. Copyright Statement: This publication may be distributed or transmitted in electronic or printed methods without permission from the publisher, the Restoration Industry Association (RIA) provided such transmission or distribution of the document is in whole, without modification, and does not contain any addition, addendum or other any other added content and is attributed to the publishers. Electronic distribution must be in the original PDF format and include all pages of the original document.